Why Does the Bottom of My Foot Hurt? A Complete Guide to Foot Pain Relief
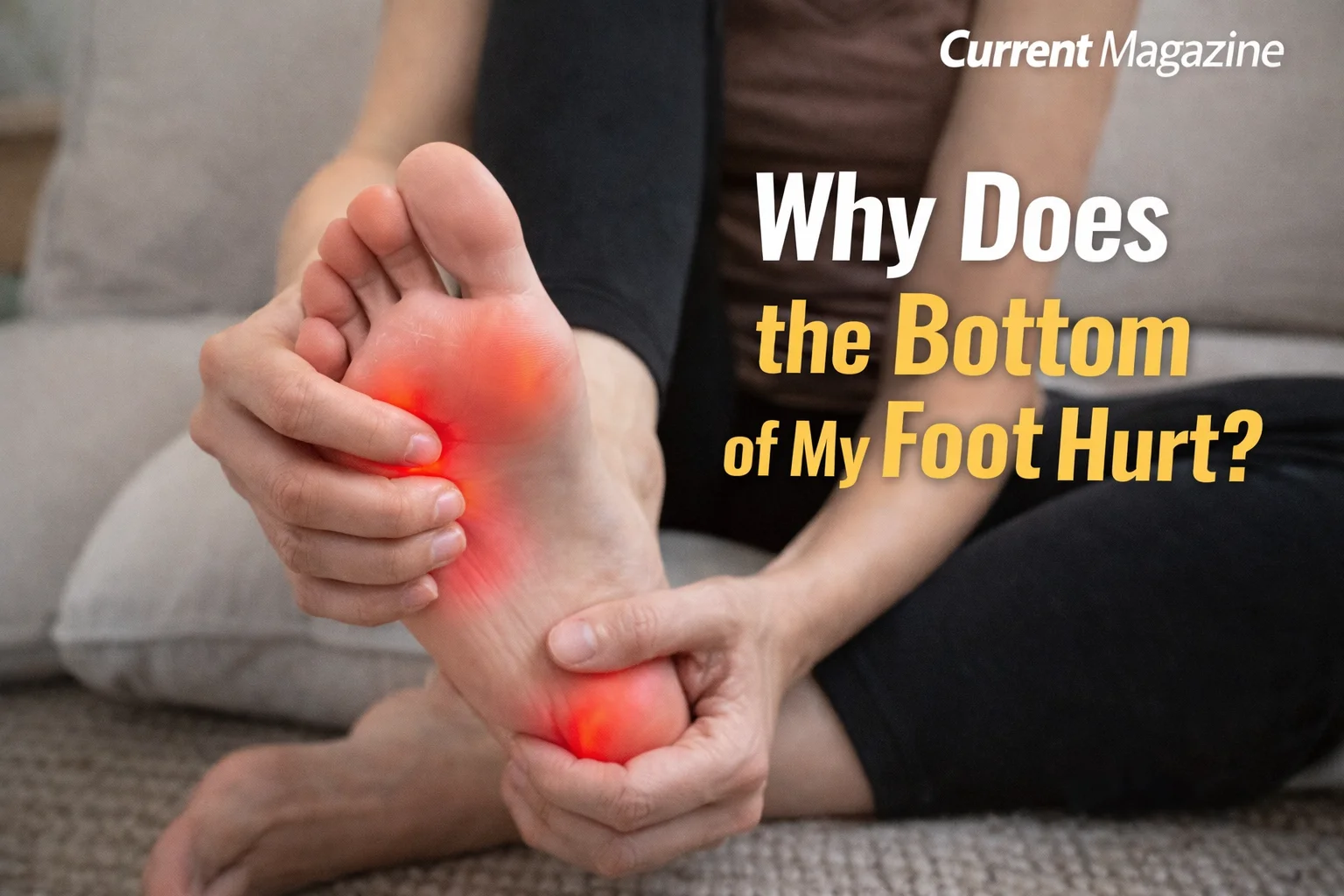
If you’re wondering “why does the bottom of my foot hurt,” you’re not alone. Bottom of foot pain, also known as plantar foot pain, affects millions of people daily and can range from a mild annoyance to severe discomfort that impacts your ability to walk. Understanding the causes of foot pain, recognizing the symptoms, and knowing when to seek treatment can help you find relief and get back to your normal activities. This comprehensive guide covers everything you need to know about pain in the bottom of the foot, including common conditions, home remedies, and prevention strategies.
Understanding Bottom of Foot Pain
The bottom of your foot, called the plantar surface, is a complex structure made up of bones, muscles, tendons, ligaments, and a thick band of tissue called the plantar fascia. This area bears your entire body weight with every step you take, making it vulnerable to various injuries and conditions. Pain in this region can occur in different areas including the heel, arch, ball of the foot, or toes, and each location often points to different underlying causes.
The pain you experience might feel sharp and stabbing, dull and achy, burning, or throbbing. It may be worse in the morning when you first stand up, after long periods of sitting, or following physical activity. Understanding your specific pain pattern helps identify the cause and appropriate treatment.
Common Causes of Bottom of Foot Pain
Plantar Fasciitis
Plantar fasciitis is the most common cause of heel and bottom of foot pain. The plantar fascia is a thick band of tissue that runs along the bottom of your foot, connecting your heel bone to your toes. When this tissue becomes inflamed or develops small tears from overuse or strain, it causes sharp, stabbing pain, typically in the heel or arch.
The hallmark symptom of plantar fasciitis is severe pain with your first steps in the morning or after sitting for extended periods. This happens because the fascia tightens during rest and then stretches suddenly when you stand, causing pain. The discomfort often improves with movement as the tissue warms up, but it may return after long periods of standing or at the end of the day.
Risk factors for plantar fasciitis include age (most common between 40-60 years), certain exercises that stress the heel (running, dancing, aerobics), foot mechanics like flat feet or high arches, obesity, and occupations that keep you on your feet for hours.
Heel Spurs
Heel spurs are calcium deposits that form on the underside of the heel bone, often developing in conjunction with plantar fasciitis. While many people with heel spurs experience no symptoms, others suffer from significant pain. The spur itself doesn’t usually cause pain; rather, the inflammation of surrounding soft tissues creates discomfort that radiates through the bottom of the foot.
Metatarsalgia
Metatarsalgia refers to pain and inflammation in the ball of your foot, the area just behind your toes where the metatarsal bones are located. This condition often feels like you’re walking on pebbles or have a bruise on the bottom of your foot. High-impact activities, ill-fitting shoes (especially high heels), foot deformities like bunions or hammertoes, excess weight, and intense training can all contribute to metatarsalgia.
Morton’s Neuroma
Morton’s neuroma is a thickening of tissue around a nerve leading to your toes, most commonly between the third and fourth toes. This condition causes sharp, burning pain in the ball of your foot and may create a sensation of standing on a fold in your sock or having a pebble in your shoe. Tingling or numbness in the toes often accompanies the pain. Tight shoes, high heels, and repetitive stress from activities like running increase your risk.
Stress Fractures
Stress fractures are tiny cracks in the bones of your feet, typically the metatarsal bones that extend from your toes to the middle of your foot. These injuries develop from repetitive force and overuse, common in runners and athletes who suddenly increase their training intensity. The pain from a stress fracture usually develops gradually, worsens with activity, and improves with rest. The affected area may be tender to touch and show swelling.
Flat Feet or Fallen Arches
Flat feet occur when the arches on the inside of your feet are flattened, allowing the entire sole to touch the floor when you stand. This condition can be present from birth or develop over time due to injury, aging, or obesity. Flat feet change the way weight distributes across your feet, often leading to pain in the arch and heel, as well as ankle, knee, and back problems.
High Arches
Conversely, unusually high arches can also cause bottom of foot pain. High arches place excessive stress on the ball and heel of the foot when walking or standing. People with high arches often experience pain, calluses, and difficulty finding comfortable shoes.
Arthritis
Several types of arthritis can affect the feet, including osteoarthritis (wear-and-tear arthritis), rheumatoid arthritis (an autoimmune condition), and gout (caused by uric acid crystal buildup). Arthritis in the foot causes pain, stiffness, swelling, and reduced range of motion. The pain often worsens in the morning or after periods of inactivity.
Peripheral Neuropathy
Peripheral neuropathy involves damage to the peripheral nerves and commonly affects the feet. Diabetes is the most common cause, but vitamin deficiencies, infections, toxins, and certain medications can also trigger it. Symptoms include burning pain, tingling, numbness, sharp or jabbing sensations, and extreme sensitivity to touch, even from the weight of a bedsheet.
Tendinitis
Tendinitis is inflammation of the tendons in your foot, most commonly affecting the Achilles tendon or the posterior tibial tendon. This causes pain, tenderness, mild swelling, and stiffness that typically worsens with activity. Overuse, sudden increase in physical activity, and improper footwear are common culprits.
Bursitis
Bursitis occurs when the small, fluid-filled sacs (bursae) that cushion the bones, tendons, and muscles near your joints become inflamed. In the foot, bursitis most often affects the heel. The pain feels like a deep, achy sensation that worsens with pressure or movement.
Bruising and Trauma
Sometimes the cause is straightforward – you stepped on something hard, dropped something on your foot, or increased your activity level too quickly. These incidents can cause bruising, inflammation, or soft tissue damage that results in pain on the bottom of your foot.
Home Remedies for Bottom of Foot Pain
Rest and Ice
When foot pain strikes, the first line of defense is often rest. Avoid activities that worsen the pain and give your foot time to heal. Apply ice to the affected area for 15-20 minutes several times daily, especially after activities. Ice reduces inflammation and numbs pain. Always wrap ice in a towel to protect your skin from cold damage.
Stretching Exercises
Gentle stretching can significantly relieve foot pain, especially for conditions like plantar fasciitis. Try these exercises:
Calf Stretches: Stand facing a wall with your hands against it. Step one foot back, keeping it straight with the heel on the ground. Bend your front knee until you feel a stretch in your back calf. Hold for 30 seconds and repeat 3-5 times on each side.
Plantar Fascia Stretch: Sit down and cross one foot over the opposite knee. Grab your toes and gently pull them toward your shin until you feel a stretch along the bottom of your foot. Hold for 30 seconds and repeat several times.
Toe Curls: Place a towel on the floor and use your toes to scrunch it toward you. This strengthens the muscles in your feet and can prevent further injury.
Proper Footwear
Wearing supportive, well-fitting shoes makes an enormous difference in foot pain. Look for shoes with good arch support, cushioning in the heel and ball of the foot, and a wide toe box. Avoid walking barefoot on hard surfaces, wearing flip-flops for extended periods, or wearing high heels regularly. Replace worn-out athletic shoes every 300-500 miles.
Orthotic Inserts
Over-the-counter arch supports and cushioned insoles can provide additional support and shock absorption. For more specific needs, custom orthotics prescribed by a podiatrist can correct biomechanical issues and redistribute pressure across your feet.
Maintain a Healthy Weight
Excess weight places additional stress on your feet with every step. Losing even a small amount of weight can significantly reduce foot pain and prevent future problems.
Over-the-Counter Pain Relievers
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can reduce pain and inflammation. Always follow package directions and consult your doctor if you need to use these medications regularly.
Night Splints
For plantar fasciitis, wearing a night splint keeps your foot in a stretched position while you sleep, preventing the plantar fascia from tightening overnight. This reduces the sharp morning pain many people experience.
Massage and Rolling
Massaging the bottom of your foot or rolling it over a tennis ball, frozen water bottle, or specialized foot roller can release tension, improve circulation, and reduce pain. Spend 5-10 minutes daily working on tight areas.
When to See a Doctor
While many cases of foot pain respond well to home treatment, certain symptoms warrant professional medical attention:
- Severe pain that prevents you from walking or bearing weight
- Pain accompanied by numbness, tingling, or color changes in your foot
- Signs of infection including redness, warmth, swelling, or fever
- Pain following an injury, especially if you heard a pop or snap
- Pain that persists for more than two weeks despite home treatment
- Diabetic patients experiencing any foot pain or changes, as they’re at higher risk for serious complications
- Deformity or inability to move your foot normally
Your healthcare provider may perform a physical examination, order imaging tests like X-rays or MRI scans, or conduct other diagnostic procedures to identify the cause of your pain. Treatment options might include prescription medications, physical therapy, corticosteroid injections, custom orthotics, immobilization in a boot or cast, or in severe cases, surgery.
Prevention Strategies
Preventing foot pain is always preferable to treating it. Here are effective strategies to keep your feet healthy:
Wear Proper Shoes: Choose supportive, well-fitting footwear appropriate for your activities. Replace worn shoes regularly and avoid going barefoot on hard surfaces.
Warm Up Before Exercise: Always warm up and stretch before physical activity, and cool down afterward. Gradually increase the intensity and duration of exercise rather than making sudden changes.
Maintain Healthy Weight: Keep your weight within a healthy range to reduce stress on your feet.
Mix Up Activities: Cross-training and varying your exercise routine prevents repetitive stress on the same structures.
Listen to Your Body: Don’t push through pain. Rest when needed and address minor discomfort before it becomes a major problem.
Strengthen Your Feet: Incorporate exercises that strengthen foot and ankle muscles into your routine.
Check Your Feet Regularly: Look for signs of problems like blisters, calluses, redness, or swelling, especially if you have diabetes or circulation issues.
Living With Chronic Foot Pain
For some people, foot pain becomes a chronic condition requiring ongoing management. Working with healthcare providers including podiatrists, physical therapists, and pain specialists can help you develop a comprehensive treatment plan. This might include regular stretching, appropriate footwear, orthotics, periodic physical therapy, and lifestyle modifications.
Staying active within your pain limits is important for overall health. Low-impact activities like swimming, cycling, or yoga can keep you fit without aggravating foot pain. Many people with chronic foot conditions find relief through consistent self-care and learning to recognize and respond to their body’s signals.
The Bottom Line
Bottom of foot pain can stem from numerous causes, ranging from simple overuse to complex medical conditions. Most cases improve with rest, proper footwear, stretching, and other home remedies. However, persistent or severe pain deserves professional evaluation to ensure proper diagnosis and treatment. By understanding what causes your foot pain and taking appropriate action, you can find relief and prevent future problems. Your feet carry you through life – taking care of them is an investment in your mobility and quality of life.
FAQs About Bottom of Foot Pain
1. Why does the bottom of my foot hurt when I wake up? Morning foot pain is most commonly caused by plantar fasciitis, which occurs when the plantar fascia tightens overnight and then stretches suddenly when you take your first steps. The fascia needs time to warm up and loosen, which is why the pain often improves after you’ve been moving for a while. Stretching before getting out of bed and wearing night splints can help reduce this morning discomfort.
2. Can dehydration cause foot pain? Yes, dehydration can contribute to foot pain, particularly muscle cramps and general achiness. When you’re dehydrated, your muscles don’t receive adequate fluids and electrolytes, making them more prone to cramping and fatigue. While dehydration alone rarely causes severe foot pain, staying well-hydrated supports overall foot health and can prevent certain types of discomfort.
3. Is it OK to walk with bottom of foot pain? This depends on the severity and cause of your pain. Mild discomfort that doesn’t worsen with walking is usually fine, but sharp, severe pain or pain that significantly worsens with activity requires rest. Walking through intense pain can worsen the underlying condition and delay healing. If you must walk, use supportive shoes, take frequent breaks, and apply ice afterward.
4. What deficiency causes foot pain? Vitamin B12 deficiency commonly causes foot pain through nerve damage, leading to tingling, numbness, and burning sensations. Vitamin D deficiency can cause bone and muscle pain in the feet, while magnesium deficiency may lead to muscle cramps and spasms. If you suspect a nutritional deficiency, consult your doctor for proper testing rather than self-diagnosing.
5. How do I know if my foot pain is serious? Foot pain is serious if you cannot bear weight, have severe swelling or deformity, notice signs of infection (redness, warmth, fever), experience numbness or tingling, or if the pain resulted from significant trauma. Additionally, pain that doesn’t improve with two weeks of home treatment or keeps you from daily activities warrants medical evaluation.
6. Can stress cause foot pain? Stress doesn’t directly cause foot pain, but it can contribute to muscle tension throughout your body, including your feet and calves. Chronic stress may also lead to behaviors that cause foot pain, like pacing, clenching your feet, or neglecting self-care. Additionally, stress can lower your pain threshold, making existing foot discomfort feel worse.
7. Why does only one foot hurt on the bottom? One-sided foot pain often results from uneven gait, favoring one leg, an injury to that specific foot, or biomechanical differences between your feet. You may unconsciously put more weight on one foot, have one foot with a different arch height, or have experienced trauma to only one side. Unilateral pain lasting more than a few days should be evaluated.
8. Does foot pain indicate diabetes? While foot pain alone doesn’t indicate diabetes, diabetic neuropathy (nerve damage from diabetes) commonly causes burning, tingling, or numbness in the feet. Diabetes also increases infection risk and slows healing. If you have unexplained foot pain along with other diabetes symptoms like increased thirst, frequent urination, or unexplained weight loss, see your doctor for testing.
9. Can flat feet be corrected? In children, flat feet often correct themselves as the arches develop. In adults, flat feet are usually permanent, but symptoms can be managed effectively with supportive footwear, custom orthotics, strengthening exercises, and proper weight management. Severe cases causing significant pain or dysfunction may benefit from surgical correction, though this is relatively rare.
10. How long does plantar fasciitis take to heal? Most cases of plantar fasciitis improve within several months with consistent home treatment, though some people experience symptoms for a year or longer. The key is maintaining a stretching routine, wearing supportive shoes, using orthotics if needed, and avoiding activities that aggravate the condition. About 90% of people recover with non-surgical treatments within 6-12 months.