What Does Gum Disease Look Like? Your Complete Visual Guide to Recognizing the Signs and Symptoms
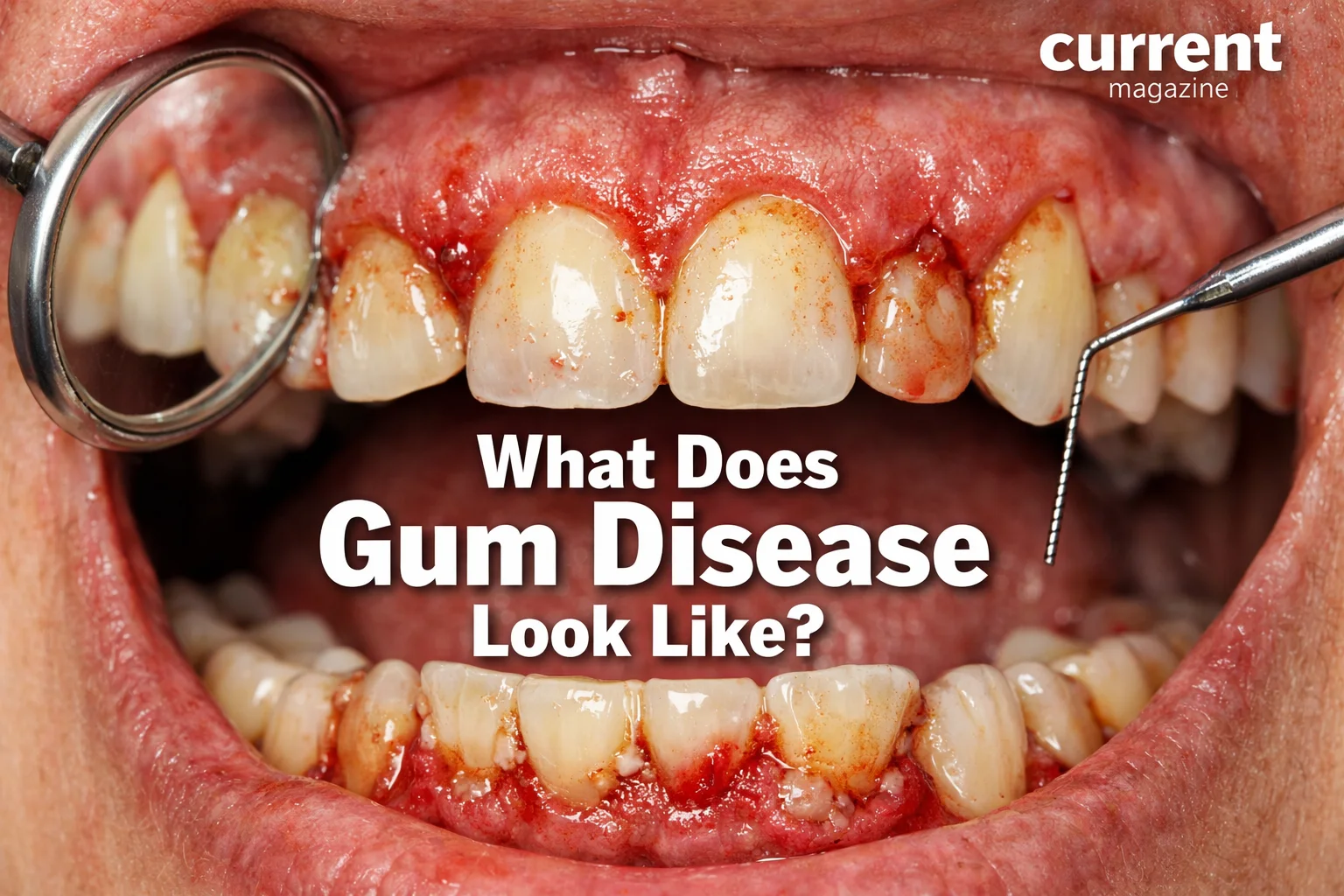
If you’re wondering what does gum disease look like, you’re taking an important step toward protecting your oral health. Gum disease (also called periodontal disease) is one of the most common dental problems affecting adults worldwide, yet many people don’t recognize the warning signs until significant damage has occurred. Understanding what does gum disease look like in its various stages can help you catch problems early when they’re easiest to treat and reverse.
Gum disease is a bacterial infection that affects the tissues surrounding and supporting your teeth. It ranges from mild inflammation called gingivitis to severe infection known as periodontitis that can destroy the bone supporting your teeth and lead to tooth loss. The appearance of gum disease changes as it progresses, with early signs being subtle and easy to miss, while advanced stages become unmistakably obvious and seriously damaging.
In this comprehensive guide, we’ll walk you through exactly what gum disease looks like at every stage, from the earliest warning signs to advanced periodontitis. We’ll describe the visual symptoms, explain what’s happening beneath the surface, share real-world comparisons to help you identify problems in your own mouth, discuss associated symptoms beyond appearance, explore risk factors, and provide actionable steps for prevention and treatment. Whether you’re experiencing symptoms yourself, concerned about a family member, or simply want to maintain excellent oral health, this detailed article will give you the knowledge you need to recognize, understand, and address gum disease.
Understanding Healthy Gums: What Normal Looks Like
Before identifying diseased gums, it’s essential to know what healthy gums should look like. This baseline helps you recognize when something’s wrong.
Characteristics of Healthy Gums
Color: Healthy gums are typically coral pink or light pink in color. The exact shade varies based on natural pigmentation—people with darker skin tones may have gums with brown or darker pigmentation, which is completely normal. The key is consistency and evenness of color.
Texture: Healthy gums have a stippled texture, often described as looking like an orange peel. The surface has tiny dots or dimples, creating a slightly textured appearance rather than being completely smooth. This texture indicates firm, healthy tissue.
Firmness: When you touch healthy gums gently, they feel firm and resilient, not soft or squishy. They hold their shape and bounce back when pressed lightly.
Shape and contour: Healthy gums fit snugly around each tooth, forming pointed triangular shapes (called papillae) between teeth. They follow the natural contours of your teeth without gaps, pockets, or recession. The gum line (where gums meet teeth) should be even and consistent.
No bleeding: Healthy gums don’t bleed during normal brushing, flossing, or eating. They can withstand the gentle pressure of oral hygiene without any blood appearing.
No swelling: Healthy gums lie flat against teeth without puffiness or swelling. There’s no inflammation that makes them bulge or appear enlarged.
No pain or tenderness: Healthy gums aren’t sensitive to touch, temperature, or normal pressure. You shouldn’t feel pain when brushing, flossing, or chewing.
Fresh breath: While breath odor can be affected by many factors, healthy gums contribute to fresh breath rather than causing bad odors.
No discharge: Healthy gums don’t produce pus or any other discharge between the gums and teeth.
Keep this healthy baseline in mind as we explore what changes occur when gum disease develops.
Stage 1: Gingivitis – What Early Gum Disease Looks Like
Gingivitis is the mildest and earliest form of gum disease. The good news is that gingivitis is completely reversible with proper treatment. Understanding what gingivitis looks like helps you catch gum disease when it’s easiest to fix.
Visual Appearance of Gingivitis
Color changes – Redness: The most noticeable early sign of gingivitis is that gums become red or bright red, especially along the gum line where gums meet teeth. Instead of healthy pink, you’ll see areas of inflammation with a reddish or purplish hue. The redness may be uniform across all gums or localized to specific areas, often between teeth or around particular teeth that harbor more plaque.
Swelling and puffiness: Gums with gingivitis appear swollen and puffy rather than firm and tight against teeth. The tissue looks enlarged and may bulge slightly. The normal triangular points (papillae) between teeth become rounded and swollen, losing their pointed shape. The gum tissue may look plump or bloated, especially along the gum line.
Shiny appearance: Instead of the healthy stippled (orange peel) texture, gums with gingivitis often look smooth and shiny. The swelling causes the tissue to stretch, eliminating the normal textural dimples. This shiny, taut appearance is a telltale sign of inflammation.
Bleeding: The most obvious functional sign is bleeding, which you’ll notice when brushing or flossing. You might see pink in the sink when you spit after brushing, blood on your toothbrush, blood on dental floss, or bleeding when eating hard or crunchy foods like apples. Even gentle pressure can cause bleeding in inflamed gums.
Tenderness: While you can’t “see” tenderness, gums with gingivitis feel sore or tender when touched. You might notice discomfort when brushing certain areas.
Plaque and tartar buildup: Gingivitis is caused by plaque (sticky bacterial film) accumulating along the gum line. You might see whitish or yellowish film along teeth where they meet gums. When plaque hardens into tartar (calculus), it appears as crusty, yellowish-brown or dark deposits, especially on lower front teeth and around back teeth.
Where Gingivitis Typically Appears First
Gingivitis often begins in areas where plaque accumulates most easily:
- Between teeth (interdental areas) where flossing is neglected
- Along the gum line, especially on lower front teeth where saliva deposits minerals
- Around back teeth (molars) that are harder to clean thoroughly
- Around crowded or crooked teeth that trap more plaque
- Near dental work like crowns, bridges, or fillings that create additional plaque traps
What’s Happening Beneath the Surface
When you see gingivitis, here’s what’s actually happening: Bacterial plaque accumulates along the gum line when brushing and flossing are inadequate. Bacteria in the plaque release toxins that irritate gum tissue. Your immune system responds with inflammation, sending more blood to the area (causing redness) and fluid (causing swelling). The inflamed tissue becomes fragile and bleeds easily because blood vessels are more exposed. However, at this stage, the infection affects only the gums—the bone and deeper structures supporting teeth remain healthy.
Why Catching Gingivitis Matters
Gingivitis is the only stage of gum disease that’s completely reversible. With improved oral hygiene and professional cleaning to remove plaque and tartar, gums can return to perfect health within days to weeks. Once gingivitis progresses to periodontitis, damage becomes permanent, making early recognition crucial.
Comparing Healthy Gums to Gingivitis
To help visualize the difference:
Healthy gums: Pale pink, firm, stippled texture, triangular points between teeth, no bleeding
Gingivitis gums: Red or purplish, swollen and puffy, smooth and shiny, rounded between teeth, bleeding when touched
Think of the difference like this: healthy gums look like a well-fitted glove snugly wrapping each tooth, while gums with gingivitis look like the glove is too big, puffy, and loose.
Stage 2: Early Periodontitis – When Gum Disease Progresses
If gingivitis goes untreated, it progresses to periodontitis—a more serious form of gum disease where infection spreads below the gum line and begins damaging the bone that supports your teeth.
Visual Appearance of Early Periodontitis
Early periodontitis includes all the signs of gingivitis plus additional warning signs:
Gum recession (pulling away from teeth): One of the hallmark signs of periodontitis is that gums begin pulling away from teeth, making teeth appear longer than before. You might notice that more of the tooth surface is exposed. The gum line becomes uneven, with some areas receded more than others. Tooth roots may start becoming visible—these appear yellowish or darker than the white crown portion of teeth because root surfaces lack enamel.
Pocket formation: As gums pull away, spaces called periodontal pockets form between teeth and gums. You can’t see these pockets directly, but you might notice that food gets stuck between teeth and gums more easily. Your dentist measures these pockets during exams—healthy pockets are 1-3mm deep, while pockets of 4mm or deeper indicate periodontitis.
Gaps between teeth: As bone loss begins, teeth may start shifting position, creating new gaps or making existing spaces larger. You might notice triangular black spaces appearing between teeth near the gum line where gums have receded.
Continued inflammation: All the signs of gingivitis persist—redness, swelling, bleeding, but often these symptoms worsen or become more persistent. Bleeding may occur with very gentle brushing or even spontaneously.
Sensitivity: Exposed tooth roots are more sensitive to hot, cold, sweet, or acidic foods and drinks. You’ll feel sharp, temporary pain when consuming these items.
Pus or discharge: In some cases, you might see yellowish or whitish pus between gums and teeth, or notice pus when pressing gently on gums. This indicates active infection.
Bad breath: Persistent bad breath (halitosis) that doesn’t improve with brushing or mouthwash often accompanies periodontitis. The odor comes from bacterial waste products and decaying tissue.
Color changes: Gums may appear darker red, purplish, or even have areas of very pale, whitish tissue where blood supply is compromised.
What’s Happening Beneath the Surface
At the early periodontitis stage: Bacteria have invaded below the gum line into periodontal pockets. These deep pockets are oxygen-poor environments where more destructive anaerobic bacteria thrive. The infection triggers your immune system to attack, but this inflammatory response actually damages your own tissues. Enzymes released during this immune battle begin breaking down collagen fibers that attach gums to teeth. Bone surrounding tooth roots begins dissolving as the infection spreads deeper. Pockets deepen as more tissue and bone are lost.
Critical Point: Irreversible Damage Begins
Unlike gingivitis, the bone loss from periodontitis is permanent. While you can stop the disease from progressing further with treatment, you cannot regenerate lost bone (except with advanced surgical procedures). This makes early detection and treatment crucial.
Measuring Progression
Dentists use a special probe to measure pocket depths:
- 1-3mm: Healthy or gingivitis
- 4-5mm: Early to moderate periodontitis
- 6mm or deeper: Advanced periodontitis
During your dental exam, if you hear your dentist or hygienist calling out numbers above 3, especially numbers of 4 or higher, this indicates periodontal pockets and gum disease progression.
Stage 3: Moderate Periodontitis – More Advanced Gum Disease
As periodontitis progresses from early to moderate stages, the visual and functional changes become more pronounced.
Visual Appearance of Moderate Periodontitis
Significant gum recession: Gums have pulled away noticeably from teeth, making them appear much longer. Large portions of tooth roots are exposed, creating an elongated appearance. The gum line is very uneven and irregular, varying significantly from tooth to tooth.
Visible bone loss: While you can’t see bone directly, you can see the effects—teeth appear to sit “higher” in the jaw with less gum and bone support. X-rays at this stage show substantial bone loss around affected teeth.
Tooth mobility: Teeth may feel loose when you touch them with your tongue or finger. You might notice teeth shifting position over time. When chewing, you may feel that teeth move slightly or feel “spongy.”
Larger gaps and spaces: Significant spaces develop between teeth as they shift. Front teeth may begin to flare outward or become crooked. The triangular black spaces between teeth become larger and more noticeable.
Deep pockets: Periodontal pockets of 6-7mm have formed, though you can’t see these depths without professional measurement. These deep pockets often collect food debris and are impossible to clean with normal brushing and flossing.
Gum tissue changes: Gums may appear very red and inflamed in some areas while looking pale or receded in others. The tissue texture is often soft and spongy rather than firm. In some areas, gums may look stringy or fibrous as healthy tissue breaks down.
Frequent bleeding and pus: Gums bleed easily with minimal contact. Pus discharge becomes more common, sometimes visible as white or yellow material at the gum line. You might taste pus or notice a bad taste in your mouth.
Exposed root surfaces: Root surfaces are clearly visible and may appear darker, yellowish, or stained. These exposed roots often have cavities (root caries) as they’re more vulnerable to decay than enamel-covered crowns.
Gum abscesses: Painful swellings may develop in gums—these appear as rounded, red or purple bumps that may ooze pus. Abscesses indicate pockets of infection and require immediate treatment.
Impact on Smile Appearance
Moderate periodontitis noticeably affects your smile’s appearance:
- Teeth look longer and more separated
- Gum line is visibly uneven and irregular
- Dark triangular spaces appear between teeth
- Teeth may look yellower as more root surface shows
- Overall smile looks “aged” as recession creates the appearance of older teeth
Functional Problems
Beyond appearance, moderate periodontitis causes:
- Difficulty chewing, especially firm or sticky foods
- Discomfort or pain when eating
- Chronic bad breath that embarrasses you socially
- Persistent bad taste in mouth
- Increased food trapping between teeth
- Sensitivity to temperature, sweetness, and pressure
What This Stage Means
Moderate periodontitis represents significant structural damage. While treatment can halt progression and even improve some symptoms, much of the lost bone and tissue cannot be fully restored without surgical intervention. The goals of treatment shift from reversal (as with gingivitis) to stabilization and prevention of further loss.
Stage 4: Advanced (Severe) Periodontitis – The Final Stage
Advanced periodontitis is the most severe form of gum disease, representing extensive destruction of the tissues and bone supporting teeth. At this stage, tooth loss is imminent without aggressive treatment, and may be unavoidable even with treatment.
Visual Appearance of Advanced Periodontitis
Severe gum recession: Gums have receded dramatically, exposing most or all of tooth roots. In severe cases, nearly the entire tooth length is visible above the gum line. The little remaining gum tissue may appear thin, fragile, and unhealthy.
Extensive bone loss: X-rays show that 50% or more of the bone supporting teeth has been destroyed. You can see the visual effects: teeth appear extremely long, teeth are positioned much higher in the jaw than normal, and the jaw itself may appear to have less bulk or definition.
Significant tooth mobility: Teeth are noticeably loose, moving when you touch them with your finger or tongue. You can feel teeth shifting when you chew or speak. In severe cases, teeth may spontaneously change position over days or weeks. Some teeth may be so loose they move or wiggle constantly.
Tooth migration and drifting: Teeth shift out of their normal positions, creating large spaces or crowding. Front teeth commonly flare outward, creating a “fan” appearance. Teeth may rotate or tilt in various directions. Your bite feels different as teeth no longer fit together properly.
Missing teeth: Some teeth may have already fallen out or been extracted due to severe looseness. Large gaps exist where teeth used to be. The loss of multiple teeth affects jaw structure and facial appearance.
Extreme pocket depths: Periodontal pockets measure 8mm or deeper in many areas. These pockets are so deep that they harbor extensive infection impossible to clean without professional intervention.
Chronic infection signs: Gums appear dark red, purple, or in some areas pale and lifeless. Pus discharge is common and may be visible without probing. Gum tissue may appear to “melt away” from teeth. Abscesses (painful pus-filled swellings) occur frequently.
Furcation involvement: In multi-rooted teeth (molars and premolars), the infection reaches the area where roots divide (the furcation). You or your dentist can actually feel or see into these areas where bone has been lost between roots. This is visible as dark openings or hollows near the gum line of back teeth.
Root exposure and damage: Large portions of tooth roots are exposed and visible. Exposed roots often have extensive cavities (root caries). Roots may appear darkly stained or damaged. In some cases, roots are partially eaten away by decay.
Gum tissue quality: Remaining gum tissue looks unhealthy—very red and inflamed or pale and fibrotic. The tissue may bleed spontaneously without any touching. Tissue texture is soft, mushy, or in some areas tough and scarred. There’s little to no attached gingiva (the firm, pink tissue that normally surrounds teeth).
Impact on Overall Appearance
Advanced periodontitis dramatically affects facial appearance and smile:
- Teeth look extremely long and “horsey”
- Smile shows large black triangular gaps between teeth
- Teeth appear crooked, tilted, or spread apart
- Missing teeth create obvious gaps
- Facial structure may look collapsed or aged where teeth are missing
- Smile looks “old” even in younger patients
- You may try to smile with lips closed to hide the appearance
Severe Functional Impairment
Advanced periodontitis severely impacts daily function:
- Chewing is difficult and painful—many foods become impossible to eat
- Speaking may be affected by loose teeth or tooth loss
- Bad breath is severe and constant, affecting social interactions
- Taste is altered by chronic infection
- Eating is limited to very soft foods
- Pain and discomfort are frequent
- Quality of life is significantly reduced
Systemic Health Connections
At this stage, the chronic infection in your mouth can affect your overall health:
- Bacteria from periodontal pockets can enter bloodstream
- Chronic inflammation affects whole body
- Increased risk of heart disease, stroke, and diabetes complications
- In pregnant women, increased risk of pregnancy complications
- Potential connections to respiratory infections and other systemic conditions
What This Stage Means
Advanced periodontitis represents severe, irreversible damage. Treatment focuses on saving as many teeth as possible, removing teeth that can’t be saved, controlling infection, and preparing for tooth replacement options (implants, bridges, dentures). Even with aggressive treatment, some tooth loss is often unavoidable. However, treatment is still essential to prevent further loss, eliminate infection, restore function, and protect overall health.
Associated Symptoms Beyond Appearance
While we’ve focused on visual appearance, gum disease causes other symptoms worth recognizing:
Pain and Discomfort
Gum tenderness: Gums feel sore when touched, brushed, or when eating.
Aching pain: Dull, persistent ache in gums or jaw, especially in advanced stages.
Sharp pains: Sensitivity to hot, cold, sweet, or acidic foods as roots become exposed.
Pressure sensitivity: Discomfort or pain when biting down or chewing, especially on loose teeth.
Abscess pain: Severe, throbbing pain if a gum abscess develops—this is a dental emergency.
Bleeding
Brushing/flossing: Blood appears when brushing or flossing—one of the earliest and most common signs.
Eating: Bleeding occurs when biting into firm foods like apples or crusty bread.
Spontaneous: In advanced cases, gums may bleed without any stimulation.
Overnight: You might wake up with blood on your pillow or notice blood in your mouth in the morning.
Bad Breath (Halitosis)
Persistent odor: Bad breath that doesn’t improve with brushing, mouthwash, or mints.
Foul taste: Constant bad taste in your mouth, often described as metallic or rotten.
Noticeable to others: People may step back during conversations or offer you mints frequently.
Morning breath worse: Bad breath is particularly bad upon waking.
Source: The odor comes from volatile sulfur compounds produced by anaerobic bacteria in periodontal pockets, plus decaying tissue and pus.
Mouth Texture and Feel
Gritty feeling: Tartar buildup creates a rough, gritty texture on teeth along the gum line.
Fuzzy teeth: Plaque makes teeth feel fuzzy or coated, especially in the morning.
Food trapping: Food gets stuck between teeth and gums much more easily.
Loose teeth: Teeth feel unstable, wobbly, or “spongy” when chewing.
Changes in bite: Teeth don’t fit together the same way when you bite down.
Systemic Symptoms
In severe cases with extensive infection:
Low-grade fever: Body responds to chronic infection with slightly elevated temperature.
Fatigue: Chronic inflammation and infection can cause persistent tiredness.
General malaise: Overall feeling of being unwell.
Swollen lymph nodes: Neck lymph nodes may be tender or enlarged as they fight oral infection.
Risk Factors and Who’s Most Susceptible
Understanding risk factors helps you assess your personal susceptibility to gum disease:
Poor Oral Hygiene
This is the number one risk factor: Inadequate brushing (less than twice daily or improper technique), infrequent or improper flossing, skipping professional dental cleanings, and allowing plaque to accumulate all directly cause gum disease.
Smoking and Tobacco Use
Tobacco is one of the most significant risk factors: Smoking impairs gum tissue healing and immune response, reduces blood flow to gums, masks symptoms (bleeding) making disease harder to detect, increases bone loss, and makes treatment less effective. Smokeless tobacco also significantly increases gum disease risk.
Genetics
Genetic predisposition plays a role: Some people are genetically more susceptible to aggressive gum disease, may have immune system variations affecting response to bacteria, or might have inherited factors affecting tissue and bone structure. If your parents or siblings have gum disease, your risk is higher.
Age
Gum disease becomes more common with age: Risk increases after age 30 and continues rising, older adults have higher prevalence due to cumulative effects of risk factors, though age itself isn’t a direct cause—older people often have had more time for disease to develop.
Diabetes
Diabetes and gum disease have a two-way relationship: Diabetes makes gum disease more likely and more severe, poorly controlled blood sugar impairs immune function and healing, and conversely, gum disease makes blood sugar harder to control. People with diabetes must be especially vigilant about gum health.
Hormonal Changes
Fluctuating hormones affect gum health, particularly in: Pregnancy (pregnancy gingivitis is common), menstruation (gums may become more inflamed before periods), menopause (decreased estrogen affects oral tissues), and puberty (hormonal changes increase gum sensitivity).
Stress
Chronic stress weakens the immune system’s ability to fight infection, may lead to teeth grinding (bruxism) that damages gums, and often correlates with poor health behaviors (neglecting oral hygiene, smoking, poor diet).
Medications
Certain medications increase gum disease risk: Drugs that reduce saliva flow cause dry mouth, allowing more bacteria to thrive. Some medications cause gum overgrowth (gingival hyperplasia) including certain blood pressure medications, anti-seizure drugs, and immunosuppressants. The overgrown tissue is harder to keep clean, trapping more plaque.
Nutritional Deficiencies
Poor nutrition compromises gum health: Vitamin C deficiency (scurvy) causes severe gum problems, calcium and vitamin D are important for bone health, other vitamins and minerals support immune function and tissue healing.
Systemic Diseases and Conditions
Various health conditions increase risk: HIV/AIDS and other immune disorders compromise infection-fighting ability, cancer and cancer treatments weaken immune response, and conditions affecting connective tissue may affect gum health.
Crooked Teeth and Dental Problems
Structural issues create plaque traps: Crowded or misaligned teeth are harder to clean thoroughly, old or defective dental work (rough fillings, poor-fitting crowns) accumulates plaque, and poorly designed or fitting dentures or bridges can irritate gums.
Family History
Beyond genetics, family patterns include: Shared environmental factors (diet, hygiene habits), learned behaviors around dental care, and similar access to dental care.
Socioeconomic Factors
Access to care affects gum health: Limited access to dental care prevents regular cleanings and early treatment, financial barriers prevent professional treatment, and health literacy affects understanding of prevention and importance of care.
The Connection Between Gum Disease Appearance and Overall Health
The way gum disease looks reflects not just oral health but can signal broader health concerns:
Cardiovascular Disease
The connection between gum disease and heart health is well-established: Bacteria from periodontal pockets can enter bloodstream and contribute to arterial plaque formation, chronic inflammation from gum disease promotes system-wide inflammation linked to heart disease, people with periodontitis have 20-30% higher risk of heart disease, and treating gum disease may improve cardiovascular outcomes.
Signs: If you have both gum disease and heart disease risk factors, the inflamed, infected appearance of your gums reflects systemic inflammation affecting your cardiovascular system too.
Diabetes
Gum disease and diabetes form a vicious cycle: Diabetes increases susceptibility to infections including gum disease, gum disease makes blood sugar harder to control, people with diabetes who develop gum disease often experience more severe, rapidly progressing disease with more dramatic visual changes.
Signs: If you have diabetes and notice rapidly progressing gum disease (quickly developing redness, swelling, recession), this may indicate poor blood sugar control.
Respiratory Infections
Oral bacteria can be aspirated into lungs: Bacteria from diseased gums can cause or worsen pneumonia and other respiratory infections, especially in elderly or hospitalized patients. This is particularly concerning in people with chronic obstructive pulmonary disease (COPD).
Pregnancy Complications
Gum disease during pregnancy is linked to: Increased risk of premature birth, low birth weight babies, and preeclampsia. Pregnancy hormones can worsen existing gum disease, creating a more inflamed, reddened appearance (“pregnancy gingivitis”).
Alzheimer’s Disease
Emerging research suggests connections: Bacteria from gum disease (particularly Porphyromonas gingivalis) have been found in brains of Alzheimer’s patients. Chronic inflammation from gum disease may contribute to neuroinflammation. More research is needed, but the association is concerning.
Rheumatoid Arthritis
Strong bidirectional relationship exists: People with RA are more likely to have gum disease, people with gum disease are more likely to develop RA, both conditions involve chronic inflammation and similar inflammatory mediators, and treating gum disease may improve RA symptoms.
Cancer
Some associations have been found: Chronic gum disease may slightly increase risk of certain cancers (pancreatic, kidney, blood cancers), though more research is needed. The connection likely involves chronic inflammation and immune dysfunction.
Osteoporosis
Bone health connections include: Systemic bone loss (osteoporosis) may correlate with jaw bone loss from gum disease, both involve similar bone metabolism pathways, and postmenopausal women with osteoporosis have higher gum disease rates.
What This Means
The inflamed, infected, damaged appearance of diseased gums isn’t just a cosmetic or dental concern—it reflects active infection and inflammation that can affect your entire body. This makes gum disease recognition and treatment important for overall health, not just dental health.
How Gum Disease Is Diagnosed
When you suspect gum disease based on appearance or symptoms, here’s how dentists confirm diagnosis:
Visual Examination
The dentist will: Look at gum color, shape, and texture, observe bleeding or pus, note recession and tooth exposure, check for swelling and inflammation, examine for plaque and tartar buildup, and assess overall oral hygiene.
Periodontal Probing
This is the gold standard for diagnosis: A small measuring instrument (periodontal probe) is gently inserted between teeth and gums to measure pocket depth. The probe has millimeter markings and is inserted around the entire circumference of each tooth. Measurements are recorded—typically six measurements per tooth (three on the cheek side, three on the tongue side). Bleeding during probing is also noted.
Interpretation:
- 1-3mm with no bleeding: Healthy
- 1-3mm with bleeding: Gingivitis
- 4-5mm: Early to moderate periodontitis
- 6mm or deeper: Moderate to advanced periodontitis
Dental X-rays
Radiographs show what’s happening beneath gums: X-rays reveal bone levels around teeth and bone loss from periodontitis (appears as dark areas where bone should be). They show the extent and pattern of bone destruction and help assess prognosis for individual teeth. Dentists typically take full-mouth x-rays every 3-5 years, with more frequent imaging if you have gum disease.
Tooth Mobility Testing
The dentist will: Gently wiggle each tooth to assess how loose it is, and grade mobility from 0 (firm) to 3 (extremely loose). Increased mobility indicates bone loss and advanced disease.
Other Assessments
Furcation involvement: In multi-rooted teeth, the dentist probes to see if infection has reached the area where roots divide.
Recession measurement: The distance from the normal gum line to the current position is measured to quantify recession.
Attachment level: The distance from a fixed point on the tooth to the bottom of the periodontal pocket is measured—this indicates the true amount of tissue attachment lost.
Medical History Review
The dentist will ask about: Medications, systemic health conditions, smoking and tobacco use, family history of gum disease, and oral hygiene habits. This helps identify risk factors and underlying causes.
Special Tests (in Some Cases)
Bacterial testing: Samples from periodontal pockets can be analyzed to identify specific bacterial species—this is sometimes done in aggressive or treatment-resistant cases.
Genetic testing: Some practices offer genetic susceptibility testing to identify patients at higher risk.
Saliva testing: Assesses overall oral bacteria levels and specific pathogenic species.
Treatment Options Based on What You See
Treatment depends on the stage and severity of gum disease:
For Gingivitis (Early Stage)
Professional cleaning: Dental hygienist removes all plaque and tartar above the gum line. This eliminates the bacterial irritants causing inflammation.
Improved home care: Brush twice daily with fluoride toothpaste for two full minutes, floss daily between all teeth, use antiseptic mouthwash if recommended, consider an electric toothbrush which can be more effective.
Timeline: With proper treatment, gingivitis resolves within 1-2 weeks. Gums return to healthy pink color, swelling disappears, bleeding stops, and tissue firms up.
Cost: Professional cleaning typically costs $75-$200, making this the most affordable stage to treat.
For Early to Moderate Periodontitis
Scaling and root planing (deep cleaning): This is a more intensive cleaning procedure where hygienist or dentist numbs your gums with local anesthetic, removes plaque and tartar from below the gum line (scaling), smooths rough spots on tooth roots where bacteria collect (root planing), and typically treats the mouth in sections over 2-4 appointments.
Antimicrobial treatments: Antibiotic gels or fibers placed in periodontal pockets, antimicrobial mouth rinses prescribed for home use, and in some cases, oral antibiotics to help control infection.
More frequent cleanings: Instead of typical 6-month cleanings, you’ll need periodontal maintenance every 3-4 months to prevent disease progression.
Improved home care: Same as for gingivitis, but even more critical to prevent progression.
Outcomes: Disease progression can be halted, inflammation and bleeding typically improve significantly, pockets may decrease in depth somewhat (though complete elimination is unlikely), but bone loss is permanent unless advanced surgical procedures are performed.
Cost: Scaling and root planing typically costs $500-$4,000 depending on severity and how many areas need treatment.
For Moderate to Advanced Periodontitis
Surgical treatments may be necessary:
Flap surgery (pocket reduction surgery): Gums are lifted back, deep tartar is removed, bone may be reshaped, gums are sutured back in place, ideally reducing pocket depths.
Bone grafting: Where bone has been destroyed, grafting materials can be placed to encourage bone regeneration and improve support for teeth.
Soft tissue grafts: Where gums have receded significantly, tissue from the palate or donor source can be grafted to cover exposed roots and improve appearance.
Guided tissue regeneration: Specialized membranes are placed to help bone and tissue regenerate.
Ongoing maintenance: Periodontal maintenance cleanings every 3 months for life are essential to prevent recurrence.
Tooth extraction and replacement: Teeth too damaged to save must be extracted and replaced with implants, bridges, or dentures.
Outcomes: Goals shift from cure to disease control—halting progression, reducing infection, improving function and comfort, and saving as many teeth as possible.
Cost: Surgical treatments range from $1,000 to $10,000+ depending on extent of disease and procedures needed.
Prevention: Keeping Gums Healthy
The best treatment is prevention. Here’s how to avoid gum disease entirely:
Essential Daily Habits
Brush properly: Brush at least twice daily (ideally after every meal), use soft-bristled toothbrush, use gentle circular motions at 45-degree angle to gum line, brush for full two minutes, don’t scrub aggressively (damages gums), replace toothbrush every 3 months, and consider electric toothbrush for more effective cleaning.
Floss daily: Floss between all teeth once daily (ideally before bed), use proper technique—curve floss around each tooth and go just beneath the gum line, be gentle to avoid cutting gums, if traditional floss is difficult, try floss picks, water flossers, or interdental brushes.
Use mouthwash: Antimicrobial mouthwash reduces bacteria, use after brushing and flossing, and choose alcohol-free formulas if you have dry mouth.
Professional Care
Regular dental cleanings: Visit dentist/hygienist every 6 months for professional cleaning and examination (more frequently if you have gum disease or risk factors). Professional cleaning removes tartar that brushing and flossing can’t.
Dental exams: Regular exams allow early detection of problems when they’re easiest to treat.
Lifestyle Factors
Don’t smoke: Quit smoking or never start—smoking is one of the most significant risk factors you can control.
Eat nutritious diet: Consume foods rich in vitamins C and D, calcium, and antioxidants. Limit sugary and starchy foods that feed bacteria. Stay hydrated to maintain healthy saliva flow.
Manage health conditions: Control diabetes with medication, diet, and lifestyle. Manage stress through exercise, meditation, or therapy. Address any systemic conditions affecting gum health.
Address risk factors: If you take medications causing dry mouth, talk to your doctor about alternatives or use artificial saliva products. If you grind teeth, get a night guard to protect teeth and gums. If you have crooked teeth making cleaning difficult, consider orthodontic treatment.
Be Vigilant
Know what healthy gums look like so you can recognize changes early.
Examine your mouth regularly: Look at your gums in the mirror, noting color, shape, and any changes.
Don’t ignore symptoms: If you notice bleeding, swelling, recession, or other warning signs, see your dentist promptly rather than waiting for your next scheduled appointment.
Act quickly on bleeding gums: Bleeding is never normal—it’s always a sign of inflammation or disease requiring attention.
When to See a Dentist Immediately
While regular checkups are essential, certain signs require prompt dental care:
Emergency Situations
Gum abscess: Painful, pus-filled swelling in gums—this indicates serious infection requiring immediate treatment (antibiotics, drainage).
Severe pain: Intense, persistent gum or tooth pain that doesn’t respond to over-the-counter pain relievers.
Fever with gum swelling: Fever combined with oral symptoms suggests serious infection that could spread systemically.
Rapidly loosening tooth: If a tooth becomes noticeably looser within days or weeks.
Trauma to gums: Injury causing significant bleeding, tears, or damage to gum tissue.
Urgent (Schedule Soon)
Persistent bleeding: Gums that bleed frequently with brushing or spontaneously.
New or worsening recession: Noticeable gum recession or increased tooth exposure.
Increasing tooth mobility: Teeth feeling looser than before.
Bad breath that won’t go away: Despite good hygiene, bad breath persists—suggests deep infection.
Changes in bite: Teeth suddenly fit together differently when you bite down.
Visible pus: Any discharge from gums.
Large swellings: Significant puffiness or swelling that doesn’t resolve within a day or two.
Why Immediate Care Matters
Early intervention for gum disease: Is always more effective and less expensive, prevents irreversible damage, saves teeth that might otherwise be lost, eliminates infection before it spreads, and improves outcomes dramatically.
Delaying treatment allows: Disease progression to more advanced stages, permanent bone loss, tooth loss, spread of infection, increased treatment complexity and cost, and potential systemic health complications.
Living With Gum Disease: Long-Term Outlook
If you’ve been diagnosed with gum disease, understanding the long-term implications and commitments helps set realistic expectations:
Gingivitis Outlook
Excellent prognosis: Gingivitis is completely reversible with proper treatment and home care. Most people achieve complete healing within weeks.
Maintenance: Continue excellent oral hygiene and regular dental cleanings to prevent recurrence.
Periodontitis Outlook
Disease can be controlled but not cured: Once you have periodontitis, you’ve permanently lost some bone and tissue support. Treatment focuses on stopping further progression.
Lifelong management required: You’ll need periodontal maintenance cleanings every 3-4 months for life, continued excellent home care, ongoing monitoring, and prompt treatment if disease flares up.
Some teeth may be lost: Despite treatment, severely affected teeth might eventually be lost and require replacement.
Treatment Success Factors
Your long-term success depends on: Compliance with professional maintenance schedule, consistent excellent home care, smoking cessation (absolutely critical), managing systemic health issues, genetic factors (some people are more susceptible to recurrence), and early intervention when problems arise.
Quality of Life
With proper management: You can keep most of your teeth for life, maintain comfortable, functional chewing, preserve your smile appearance, prevent pain and infection, and protect your overall health.
Without proper management: Progressive tooth loss, pain and discomfort, difficulty eating, embarrassment about appearance and breath, and potential systemic health complications all become likely.
Financial Considerations
Gum disease requires ongoing investment: Maintenance cleanings 3-4 times yearly ($100-$200 per visit), potential additional treatments if disease progresses, possible tooth replacement costs (implants $3,000-$6,000 each, bridges $2,000-$5,000, dentures $1,000-$8,000+).
Prevention is far less expensive than treatment: Regular cleanings twice yearly ($75-$200) and good home care products ($100-$200 annually) cost far less than treating advanced disease.
Emotional and Social Impact
Gum disease can affect: Self-confidence due to appearance changes, social interactions if you’re self-conscious about breath or appearance, and quality of life if eating becomes difficult or painful.
Successful treatment improves: Confidence and self-esteem, comfort and function, and social relationships.
Conclusion: The Importance of Recognizing Gum Disease
Understanding what gum disease looks like empowers you to protect your oral health. The visual signs—from the early redness and swelling of gingivitis to the severe recession, mobility, and infection of advanced periodontitis—tell an important story about what’s happening in your mouth.
Key Takeaways:
Healthy gums are pink, firm, and don’t bleed. Any deviation from this baseline deserves attention.
Gingivitis (early stage) appears as red, swollen, shiny gums that bleed easily. This stage is completely reversible with proper care.
Periodontitis shows as gum recession, tooth lengthening, gaps between teeth, looseness, and persistent infection. This stage causes permanent damage but can be controlled with treatment.
Advanced periodontitis looks severe—extreme recession, very loose teeth, visible bone loss, chronic infection, and tooth loss. Aggressive treatment is needed to save any teeth.
Early detection is crucial. The earlier you catch gum disease, the easier, less expensive, and more effective treatment becomes.
Regular dental visits are essential because professionals can detect early changes you might miss and provide treatment before damage becomes severe.
Prevention is possible. Good oral hygiene, regular professional care, not smoking, and managing health conditions prevent most gum disease.
Gum disease affects overall health, not just your mouth. The infection and inflammation visible in diseased gums can impact cardiovascular health, diabetes control, pregnancy outcomes, and more.
Treatment is always worthwhile, no matter what stage. Even advanced disease can be managed to prevent further loss and improve quality of life.
If you recognize any signs of gum disease in your own mouth—bleeding gums, redness, swelling, recession, looseness, or any other symptoms discussed in this article—don’t wait. Schedule a dental appointment promptly. Early intervention can save your teeth, protect your health, and preserve your smile for a lifetime. Your gums are the foundation of your oral health—take care of them, and they’ll take care of you.
10 Frequently Asked Questions About What Gum Disease Looks Like
1. Can gum disease go away on its own without treatment?
Gingivitis, the earliest stage of gum disease, can improve significantly with better oral hygiene alone, but it rarely resolves completely without professional intervention. If you notice early signs like redness, swelling, or bleeding and immediately improve your brushing and flossing technique, you may see noticeable improvement within days. However, once tartar (hardened plaque) has formed along the gum line, you cannot remove it with brushing alone—professional cleaning is necessary to eliminate it completely. Without removing tartar, the bacterial irritation continues and gum disease persists or worsens. Once gum disease progresses to periodontitis (with bone loss and deep pockets), it absolutely cannot reverse on its own. Periodontitis requires professional treatment including deep cleaning (scaling and root planing) and possibly surgery. The bone loss from periodontitis is permanent and cannot regenerate without advanced procedures. Even with treatment, periodontitis requires lifelong professional maintenance to prevent recurrence—it’s a chronic condition requiring ongoing management. The bottom line: While very early gingivitis might improve somewhat with better home care, proper treatment always requires professional cleaning to remove tartar and ensure complete resolution. Periodontitis always requires professional treatment and never resolves on its own. Waiting and hoping gum disease will disappear is risky—it allows progression to more advanced, irreversible stages.
2. Is it normal for gums to bleed a little when brushing, or does this always mean gum disease?
Bleeding gums are never normal—they always indicate some degree of inflammation or disease, even if it’s very mild. Healthy gums do not bleed from gentle brushing or flossing. The most common cause of bleeding gums is gingivitis (early gum disease) caused by plaque accumulation along the gum line. When bacteria irritate gum tissue, it becomes inflamed, engorged with blood, and fragile, bleeding easily when disturbed. However, other causes of bleeding gums include brushing too hard with a hard-bristled toothbrush (this damages tissue), trauma from aggressive flossing or toothpicks, medications that thin your blood (like aspirin or warfarin), vitamin deficiencies (particularly vitamin C deficiency), hormonal changes during pregnancy or menstruation, bleeding disorders (rare), and new oral hygiene routines (when you first start flossing, gums may bleed for a few days before improving). If your gums bleed occasionally during brushing, especially if you haven’t been flossing regularly and just started, this typically indicates mild gingivitis. Improve your oral hygiene with gentle, thorough brushing twice daily and daily flossing. If bleeding doesn’t stop within 1-2 weeks of consistent good hygiene, see your dentist. If gums bleed frequently, spontaneously, or heavily, see your dentist promptly as this suggests more significant gum disease or other problems. Never ignore bleeding gums—they’re your body’s way of signaling that something is wrong. The earlier you address it, the easier treatment becomes.
3. What’s the difference between gum disease and gum recession—are they the same thing?
Gum recession and gum disease are related but not identical. Gum recession is a symptom or consequence of gum disease (periodontitis), but it can also occur from other causes. Gum recession refers specifically to the gum tissue pulling away from teeth, exposing more of the tooth surface and potentially the root. It’s a physical change in gum position. Gum disease (periodontitis) is an infection and inflammation of the gums and supporting structures that destroys bone and tissue, often causing recession as one of its symptoms. Here’s how they relate: Periodontitis is the most common cause of gum recession—as infection destroys supporting structures, gums pull away from teeth. However, gum recession can also result from aggressive brushing with hard-bristled toothbrushes (mechanical trauma), genetics (some people naturally have thin, delicate gum tissue that recedes easily), orthodontic treatment (tooth movement can cause recession), tobacco use, teeth grinding (bruxism), and lip or tongue piercings that rub against gums. So while gum disease commonly causes recession, not all recession is from gum disease. Distinguishing factors: Recession from periodontitis typically appears with other signs—redness, swelling, bleeding, deep pockets, bone loss on X-rays, and affects multiple teeth. Recession from aggressive brushing usually appears on prominent teeth (canines, first molars) where you brush hardest, without signs of infection. The treatment differs too: periodontitis-related recession requires infection control, deep cleanings, possibly surgery; recession from mechanical causes requires correcting brushing technique and may benefit from gum grafting to cover exposed roots. If you notice recession, see your dentist to determine the cause and appropriate treatment.
4. Can gum disease make my teeth fall out, and how long does this take?
Yes, gum disease is the leading cause of tooth loss in adults. The timeline from early gum disease to tooth loss varies dramatically based on disease severity, type of bacteria involved, your immune response, whether you smoke, systemic health factors like diabetes, and most importantly, whether you receive treatment. For untreated gum disease: Gingivitis can persist for months or years without progressing (though it often does progress). Early to moderate periodontitis might take 5-10 years or longer to cause tooth loss in slow-progressing cases. Aggressive periodontitis can cause severe bone loss and tooth mobility within months to a few years. Advanced periodontitis with extensive bone loss can result in tooth loss within weeks to months once teeth become very loose. The process of tooth loss from gum disease: Bacteria accumulate in plaque along the gum line, irritating gums and causing gingivitis. Without treatment, infection spreads below the gum line (periodontitis begins). Bacteria release toxins; your immune system responds with inflammation. The inflammatory process destroys collagen fibers attaching gums to teeth and dissolves bone supporting teeth. As bone dissolves, teeth lose their structural support. Teeth gradually become loose as they lose bone support. Eventually, teeth become so loose they fall out spontaneously or must be extracted. Critical point: This entire process can be halted at any stage with proper treatment. If you catch and treat gingivitis, no permanent damage occurs. If you treat early periodontitis, you can prevent further bone loss and maintain your teeth for life (though lost bone won’t regenerate without surgical procedures). Even advanced periodontitis can often be managed to save many teeth with aggressive treatment. The key is early intervention—the earlier treatment begins, the more teeth you’ll keep. If you notice signs of gum disease, don’t wait to see if teeth will fall out—seek treatment immediately to prevent this outcome.
5. I have red, swollen gums but they don’t hurt—should I still be concerned?
Yes, you should absolutely be concerned about red, swollen gums even if they don’t hurt. Gum disease is often painless in its early and moderate stages, which is one reason it’s so common and often goes unnoticed until significant damage has occurred. The absence of pain doesn’t mean absence of disease—it means the disease hasn’t progressed to the point of causing nerve pain or hasn’t caused acute infection (abscess). Here’s what red, swollen, painless gums likely indicate: This is classic gingivitis or early periodontitis. The redness indicates increased blood flow from inflammation. Swelling shows tissue edema (fluid accumulation) from immune response. The lack of pain occurs because gums don’t have many pain nerve endings and because chronic, low-grade infection often doesn’t trigger pain receptors the way acute infection does. Why painless disease is dangerous: Without pain to motivate action, people often ignore symptoms and delay treatment. The disease progresses silently, destroying bone and tissue. By the time pain develops, significant irreversible damage has usually occurred. Pain typically only appears when acute infection develops (abscess), when recession exposes sensitive tooth roots, when loose teeth create pressure sensitivity, or when advanced disease affects deeper structures. What you should do: Red, swollen gums require dental evaluation and treatment even without pain. The treatment at this stage is simple—professional cleaning and improved home care. Waiting until pain develops means the disease has progressed to more advanced, difficult-to-treat stages requiring expensive procedures. Think of it this way: high blood pressure doesn’t hurt either, but you still treat it because it causes serious damage. Gum disease is similar—painless doesn’t mean harmless. Schedule a dental appointment as soon as you notice red or swollen gums, regardless of whether they hurt.
6. Are white gums a sign of gum disease, or is this something else?
White gums are not a typical sign of gum disease, which usually causes red or purple discoloration. White gums usually indicate different conditions and warrant dental evaluation to determine the cause. Common causes of white gums include: Leukoplakia—thick, white patches that can’t be scraped off, often caused by chronic irritation (from tobacco, cheek biting, rough tooth edges, or ill-fitting dentures). Most patches are benign but some can be precancerous, requiring monitoring or biopsy. Oral thrush (candidiasis)—fungal infection causing white, cottage-cheese-like patches that can be wiped away, leaving red, sometimes bleeding tissue underneath. Common in people with weakened immune systems, diabetes, or after antibiotic use. Lichen planus—autoimmune condition causing white, lacy patterns on gums and inside cheeks, sometimes with redness and sores. Oral lichen planus requires monitoring. Anemia—severe anemia can cause pale, whitish gums due to reduced blood flow and low red blood cell counts. Canker sores (aphthous ulcers)—small, painful white or yellowish ulcers with red borders, usually inside lips or cheeks but sometimes on gums. When white gums accompany gum disease: In advanced periodontitis, some areas of gum tissue might appear pale or whitish due to poor blood supply from destroyed tissue, but this usually occurs alongside typical red, inflamed areas elsewhere. Gum abscesses might have whitish or yellowish areas where pus collects. What to do: White patches or pale gums require dental examination to diagnose the cause. Some causes (like leukoplakia) need biopsy to rule out cancer. Others need specific treatments (antifungal for thrush, managing underlying conditions for lichen planus or anemia). Don’t try to self-diagnose based on color alone—let your dentist examine the tissue, evaluate the pattern and distribution, and determine appropriate next steps.
7. Can children get gum disease, and what does it look like in kids?
Yes, children can definitely get gum disease, though it’s less common than in adults. The appearance and causes differ somewhat from adult gum disease. Types of gum disease in children: Gingivitis is fairly common in children, especially during puberty when hormonal changes increase gum sensitivity to plaque. It looks similar to adult gingivitis—red, swollen gums that bleed when brushing. Aggressive periodontitis (now called “periodontitis in young patients” under new classification) is rare but serious. It can affect children and teenagers, causing rapid bone loss. It often affects specific teeth (incisors and first molars) rather than all teeth. What pediatric gum disease looks like: In young children with gingivitis: Puffy, swollen gums that may appear redder than healthy pink gums, bleeding when brushing teeth or eating, bad breath unusual for a child. In aggressive periodontitis: More dramatic symptoms including rapidly loosening teeth, gum recession making teeth look longer, gaps developing between front teeth as they shift, visible pus or infection, pain or discomfort, and sometimes systemic symptoms like fever or swollen lymph nodes. Common causes in children: Poor oral hygiene (children often don’t brush thoroughly), orthodontic braces (make cleaning more difficult, create more plaque traps), mouth breathing (dries out gums, increasing inflammation), diabetes or other systemic conditions, genetic predisposition (some children are more susceptible), and rarely, conditions affecting immune function. Why children’s gum disease matters: Baby teeth are temporary, but gum disease can affect the supporting bone that will hold permanent teeth. Habits and oral health patterns established in childhood continue into adulthood. Aggressive periodontitis can cause permanent tooth loss in young people. Early gum disease might signal systemic health problems requiring investigation. What parents should do: Ensure children brush twice daily with fluoride toothpaste (use pea-sized amount for children under 6), help young children brush until they develop proper technique (usually around age 7-8), floss children’s teeth daily once teeth touch, limit sugary snacks and drinks, and take children for regular dental checkups starting by age 1. If you notice red, swollen, or bleeding gums in your child, see a pediatric dentist or family dentist promptly.
8. How quickly can gum disease progress from early to advanced stages if left untreated?
The progression rate of gum disease varies enormously between individuals and depends on multiple factors. There’s no single timeline—progression can be very slow or alarmingly fast. Factors affecting progression speed: Bacterial species involved—some bacteria are more aggressive than others. Immune system function—some people’s immune responses inadvertently cause more tissue destruction. Smoking accelerates progression dramatically. Genetics play a significant role—some people are genetically predisposed to rapid progression. Systemic health conditions like diabetes accelerate disease. Stress and poor nutrition affect progression. Oral hygiene quality—even with disease, good hygiene slows progression. Typical progression patterns: Chronic periodontitis (most common type, affects older adults): This typically progresses slowly over many years. Gingivitis might persist for years without progressing (though it often does). Once periodontitis begins, progression might be 0.5-1mm of bone loss per year without treatment. At this rate, it might take 10-20+ years to cause severe bone loss and tooth loss. However, progression isn’t linear—there may be periods of stability followed by bursts of active disease. Aggressive periodontitis (less common, affects younger people): This can progress extremely rapidly. Bone loss might be 2-3mm or more per year. In severe cases, teenagers or young adults can lose significant bone support within just a few years. Tooth loss can occur within months to a few years without treatment. Real-world examples: A person with slow chronic periodontitis might have mild gingivitis at age 30, moderate periodontitis at age 45, and advanced periodontitis at age 60 without treatment. Someone with aggressive disease might develop moderate periodontitis in their 20s and face tooth loss by their 30s. A smoker with diabetes might progress from gingivitis to severe periodontitis in just 5-10 years. The unpredictability factor: Because progression is so variable and unpredictable, waiting to see “how fast it progresses” is risky. Some people are lucky and have slow progression, but you don’t know if you’re in that group. Once periodontitis begins, bone loss is permanent (barring surgical intervention). The safest approach: Treat any gum disease as soon as it’s detected, regardless of how slow or fast you think it might progress. Don’t gamble with your teeth.
9. Can gum disease be reversed, or is the damage permanent once it starts?
The answer depends entirely on what stage gum disease has reached. Gingivitis is completely reversible. With professional cleaning to remove plaque and tartar and improved oral hygiene at home, inflamed gum tissue returns to complete health within 1-2 weeks. The gums return to healthy pink color, swelling disappears, bleeding stops completely, and tissue firms up. No permanent damage occurs from gingivitis if treated properly. Periodontitis damage is permanent—but progression can be stopped. Once periodontitis develops, certain changes cannot be fully reversed: Bone loss is permanent (bone that’s been destroyed by infection doesn’t regenerate spontaneously). Attachment loss (where gum and ligament fibers detach from teeth) is generally permanent. Recession (gums that have pulled away) doesn’t spontaneously reattach to their original position. However, treatment can: Halt disease progression completely, eliminate infection and inflammation, reduce pocket depths somewhat (though not usually to normal), prevent further bone loss, maintain remaining teeth and supporting structures, and in some cases, with advanced surgical techniques, regenerate some lost bone and tissue. Advanced surgical options: For periodontitis, certain procedures can partially reverse damage: Guided tissue regeneration uses membranes and bone grafts to encourage some bone regrowth. Soft tissue grafts can cover exposed roots and restore gum tissue. Bone grafting can restore some lost bone in favorable cases. However, even with these procedures, you typically can’t achieve complete restoration to pre-disease state. The extent of possible regeneration is limited and unpredictable. The practical answer: Gingivitis: 100% reversible—treat it immediately and you’ll be completely fine. Early periodontitis: Partially reversible with advanced treatments, but practically speaking, damage control and stabilization are realistic goals. Advanced periodontitis: Damage is extensive and permanent; treatment focuses on saving what remains. Key message: This is why early detection and treatment are so critical. If you catch disease at the gingivitis stage, you can reverse it completely. Once it progresses to periodontitis, you’re managing a chronic condition rather than curing it. Don’t wait—act on early signs immediately.
10. If my gums look healthy but I haven’t been to the dentist in years, could I still have gum disease?
Yes, absolutely. Gum disease can be present even when gums appear relatively normal to the untrained eye, and there are aspects of gum disease that only professional examination can detect. Here’s why you might have gum disease despite gums looking okay: Early periodontitis can be subtle: Deep periodontal pockets form below the gum line where you can’t see them. The visible gum tissue might look fairly normal while hidden pockets harbor infection. Initial bone loss isn’t visible to the naked eye—only X-rays reveal it. Some people’s gums don’t show obvious inflammation (redness, swelling) despite active disease. You might be missing subtle signs: Gum disease starts very gradually with subtle changes easy to overlook if you don’t know what to look for. You might have adapted to gradual changes (slight recession, color changes) without realizing they’re abnormal. Without comparing to professional standards, you might think your gums are fine when a dentist would immediately identify problems. Smoking masks symptoms: Smokers often have less obvious gum inflammation and bleeding because nicotine constricts blood vessels. This creates a false impression of gum health while disease progresses underneath. Smokers can have advanced periodontitis with less visible redness and swelling than non-smokers with the same disease level. Professional examination detects hidden disease: Periodontal probing measures pocket depths you can’t assess at home. Pockets of 4mm or deeper indicate disease even if gums look okay on the surface. X-rays show bone loss invisible to visual inspection. Dentists recognize subtle color, texture, and contour changes that untrained eyes miss. Professional judgment accounts for your age, medical history, risk factors, and overall oral health. What happens without regular checkups: Gradual disease progression goes unnoticed and unchecked. By the time symptoms become obvious enough for you to notice, disease has often reached moderate or advanced stages. Opportunities for early, simple, reversible treatment are missed. The bottom line: You cannot accurately assess your periodontal health by looking in the mirror at home. Even if your gums look fine to you, regular professional examinations are essential because dentists have tools, training, and techniques to detect disease you can’t see. If you haven’t had a professional examination in years, you’re at risk for undetected gum disease. Schedule an appointment for a comprehensive examination including periodontal probing and X-rays. Even if everything looks fine to you, professional evaluation is the only way to truly know your periodontal health status.